Information Links
Related Conferences
Current Issue Volume 10, Issue 3 - 2025
Etiology and Pathogenesis of Inflammatory Diseases of the Biliary Tract: A Hypothesis
Michael D Levin*
Dorot. Medical Center for Rehabilitation and Geriatrics, Netanya, Israel
*Corresponding Author: Michael D Levin, MD, Ph.D, Dorot. Medical Center for Rehabilitation and Geriatrics, Department of Pediatric Radiology of the 1-st State Hospital, Minsk, Belarus, Dorot. Medical Center for Rehabilitation and Geriatrics, Amnon veTamar, Netanya, Israel, Tel: 972-538281393, Email: [email protected]
Received Date: November 25, 2025
Published Date: December 26, 2025
Citation: Levin MD. (2025). Etiology and Pathogenesis of Inflammatory Diseases of the Biliary Tract: A Hypothesis. Mathews J Gastroenterol Hepatol. 10(3):37.
Copyrights: Levin MD. © (2025).
ABSTRACT
All articles devoted to the pathology of the biliary tract provide risk factors, which are listing clinical, histological, and other characteristics associated with acute and chronic cholecystitis with and without stones, as well as with acute obstructive cholangitis. These factors are unrelated to the etiology of the disease; however, the causes of biliary tract pathology are not given at all. Each nosologically entity is described as a separate disease, as if gallbladder dyskinesia and cholelithiasis are not stages of pathogenesis. We analyzed the literature and our own research to determine the etiology and pathogenesis of biliary system diseases. We provide evidence that biliary pathology arises from hydrochloric acid hypersecretion. Therefore, it is associated with other acid-dependent diseases, including gastroesophageal reflux disease and inflammation (ulcers) of the stomach and duodenum. Hypersecretion of hydrochloric acid causes dyskinesia of the sphincter of Ochsner, leading to increased pressure in the duodenum, where the sphincter of Oddi opens. This leads to increased pressure in the common duct and its dilation, stagnation of bile in the gallbladder, increased bile concentration, and stone formation. Dysfunction of the sphincter of Oddi and the common duct leads to periodic reflux of duodenal chyme and bacteria into the bile ducts. The disease progresses from dyskinesia to stone formation and acute inflammation. Stone formation and symptoms are most often observed after age 40, as dyskinesia can present asymptomatically or overlap by symptoms of other acid-related diseases. Discussion of this hypothesis will help select more rational methods for diagnosing and treating biliary tract pathologies.
Keywords: Hydrochloric Acid Hypersecretion, Biliary Tract Pathology, Cholecystitis, Gallstones, Sphincter Oddi Dysfunction, Sphincter Ochsner Dyskinesia, Etiology and Pathogenesis.
INTRODUCTION
Twenty to 25 million Americans have gallstones. Annually, more than 750,000 individuals undergo cholecystectomy in the United States. Cholecystolithiasis accounts for 90%–95% of all causes of acute cholecystitis, while acalculous cholecystitis accounts for the remaining 5%–10% [1,2]. All authors of articles list many factors that have been linked to gallbladder disease under the concepts of etiology and pathogenesis. These risk factors represent a list of clinical, histological, and other characteristics associated with acute and chronic cholecystitis with and without stones, as well as with acute obstructive cholangitis. For example, for gallstone disease risk factors include unmodifiable i.e., aging, female gender, races, and lithogenic (LITH) genes and modifiable conditions (metabolic syndrome, dietary factors, increased enterohepatic circulation of bilirubin, medications, defective gallbladder motility) [3]. However, these factors are unrelated to either etiology or pathogenesis. To prevent the pathological process and effectively treat the disease, it is necessary to understand why it occurs in certain groups of people and not in others. For example, it is known that the bile of healthy subjects is generally aseptic [3]. Therefore, it is necessary to determine how the microbes enter the gallbladder. The assertion that acute calculous cholecystitis is caused by bile duct obstruction by a stone requires an explanation of how the stone formed in the gallbladder. An article by Ochsner (1906) clarified the pathogenesis of acid-related diseases. During gallbladder and stomach operations Ochsner found the duodenum is distended with gas to a point just below the entrance of the common duct, while below this it is contracted. In all histological specimens, there was also a marked thickening of the intestinal wall for 2 to 4 centimeters below entrance of the common duct, with an increase in the circular fibers. Ochsner first described the sphincter in the third part of the duodenum. He believed that this sphincter contracts in response to hydrochloric acid to prevent the passage of a low-pH bolus into the jejunum. In acid-related diseases such as gastric and duodenal ulcers, hypersecretion of hydrochloric acid causes hypertrophy of the sphincter walls, leading to biliary tract pathology [4].
The aim of this study, based on a literature review and our own research, is to determine the etiology and pathogenesis of inflammatory diseases of the biliary tract.
The stomach is a chemical reactor that secretes hydrochloric acid and pepsin, breaking down food into small particles that can be absorbed in the intestine. To prevent the destructive force of gastric chyme from damaging the digestive tract, the stomach and duodenal bulb have rapidly changing mucosa. Sphincters of the duodenum play an important role in maintaining normal function, and the sphincter of Oddi (SO) is one of them. This sphincter is located on the border between the bile, and pancreatic ducts on one side and the duodenum on the other. It regulates the portioned flow of bile and pancreatic juice into the duodenum. Secondly, it prevents the reflux of duodenal contents into the ducts [5].
Normal anatomy and physiology of the SO
In most cases, the common bile duct connects close to the duodenum with the large pancreatic duct, forming a common canal that flows into the duodenum. The terminal part of this canal, called the greater duodenal nipple or papilla Vateri, is in the lumen of the duodenum. Circular smooth muscle fibers of the SO surround the lower portion of the common bile duct, of the large pancreatic duct, and the common duct (Figure 1. а) [6]. Kune was the first to show that the zone of narrowing of the distal segment of the common duct, when studied with X-ray contrast agents, represents a zone of active contraction of the SO, which can be measured [7] (Figure 1, b, c).
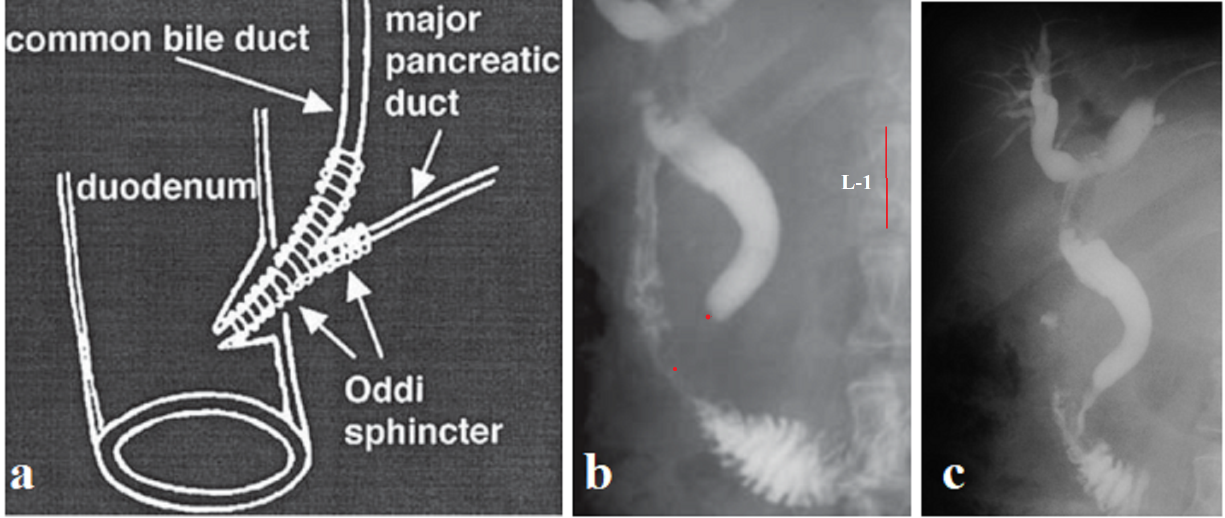
Figure 1. Towards the anatomy of SO. (a) Diagram from the article by Geenen et al [3]. (b, c). Stages of cholecysto-cholangiography in an elderly patient with SO dysfunction. (b). Since it is known that the height of the 1st lumbar vertebra in adults is approximately 2.2 cm, the distance between the two red dots, which is caused by the contraction of SO, is 1.1 cm. The width of the CBD in the proximal part is 1 cm, and above the SO - 0.5 cm. The straightened contours of the 2nd part of the duodenum indicate duodenitis. (c). The contrast agent passes into the duodenum through SO.
Since contrast studies are performed only on patients, the results of measuring SO length by this method should be treated with caution. In a manometric study, SO length was, in the control group, 9.5 ± 0.5 mm. No significant differences were found between controls and patients with common bile duct (CBD) stones [8]. Funch-Jensen et al during endoscopic manometry in healthy volunteers identified SO as a zone with elevated base-line pressure with an average length of 8 mm [9]. These studies of the SO anatomy were carried out in the 20th century. In all articles, SO is described as a narrow channel with a length of about 9.5 ± 0.5 mm [8]. This size is probably closer to the truth, since this was the only study conducted among control subjects. SO generates a basal pressure that is higher than the pressure in the common bile duct and duodenum. In healthy volunteers, median values for amplitude were 102.9 mm Hg; base-line pressure, 10 mm Hg; wave duration, 4.8 sec; and frequency, 2.6/min. Most waves propagated antegrade or simultaneously, and in no individual were more than one third of the waves retrograde [9]. The results of determining the length of the common bile duct and its tone, measured by the hydraulic capillary infusion system and a triple-lumen catheter, can be considered acceptable. However, determining the direction of peristalsis in the common bile duct contradicts the law of intestine by Bayliss and Starling, which was described 126 years ago and has not been refuted to this day. It also does not correspond to physiological necessity. The error is because the catheter obstructs the lumen of the common bile duct, causing its contraction in response to irritation. The peristaltic wave, upon encountering an obstruction, is thrown back retrograde. This is also facilitated by infusion directed against antegrade peristalsis.
What is a SO ampulla?
In recent decades, a completely different picture has been described as normal SO anatomy. During cholangiography, in the area between the CBD and the papilla, two areas of contraction are identified, between which there is a wide cavity called the ampulla. When the peristaltic wave reaches SO, “first the upper part, the sphincter choledochus, opens from above downwards, the contrast enters the ampulla. Then the sphincter choledochus contacts, again from above downwards, isolating a small portion of contrast in the ampulla. The distal sphincter opens, and the systolic volume falls into the duodenum” [10]. These authors, examining serious patients who required cholangiography, have no reason to consider the obtained results as anatomically normal. It is sufficient to compare the radiographs in Figure 1bc with the radiograph in Figure 2a to see that the ampulla is combined with a sharp dilation of the common duct. The ampullae appears in all sphincter zones, if sphincters function impaired. Normally, the last peristaltic wave creates threshold pressure for sphincter opening. The ampulla represents the last peristaltic wave in a wide bore channel, which reduces its ability to create threshold pressure for SO opening. To create a threshold pressure, a functional sphincter arises, and it contraction allows the ampulla to create a higher pressure and inject a bolus into the lumen with a higher pressure than in the CBD (Figure 2. a, b) [11].
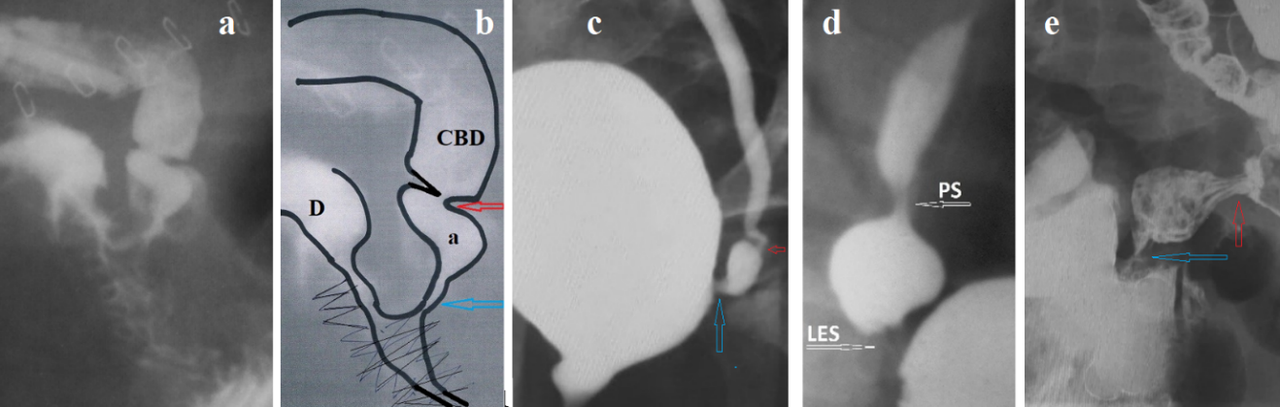
Figure 2. (a) Cholangiography for severe SO damage, and (b) a diagram for it. (d – duodenum; CBD – common bile duct; a – ampulla located between the shortened SO - blue arrow, and the functional sphincter - red arrow). (c) Vesicoureteral reflux. The ampulla is located between the vesicoureteral sphincter - blue arrow, and the functional sphincter - red arrow. (d) Gastroesophageal reflux. The phrenic ampulla is located between the LES and the functional (proximal) sphincter (PS). (e). A patient with enteritis. The ampulla is located between the ileocecal valve - blue arrow, and the functional sphincter - red arrow.
It follows that the presence of an ampulla is evidence of severe SO damage.
Since the antireflux function of SO depends on the condition of the duodenum, below we will dwell on the normal anatomy and physiology of the duodenum.
Duodenal motility
In the duodenum, four sphincters function, which protects the small intestine from the aggressive effects of hydrochloric acid. If the bolus passed through the duodenum as quickly as it passed through the esophagus, the extremely low pH bolus could cause damage to the jejunum. The post bulbar sphincter (PBS), together with the pyloric sphincter (PS), provides evacuation of the chyme from the stomach as portions of a certain volume (Figure 3 A). When the acid bolus reaches the Ochsner’s sphincter, which is in the 3rd part of the duodenum, it causes its contraction, which prevents entering aggressive chyme to the jejunum (Figure 3 B). As a result of the Ochsner’s sphincter contraction, the bolus is thrown cranially, but Kapanji’s sphincter contraction [12], bolus is again thrown в towards the Ochsner’s sphincter. This pendulum movement of the bolus between the Ochsner and Kapanji sphincters occurs several times. During this time, the chyme mixes with bile and pancreatic juice, which raises the pH of the chyme. When the pH reaches a level that is safe for the jejunum, Ochsner’s sphincter opens, and bolus passes into the jejunum [4, 12,13,14]. On a standard x-ray study, barium passes through the duodenum without delay because it has a high pH. When vitamin “C” was added to barium, we found a contraction of the Ochsner and Kapandji sphincters and were able to determine their sizes (Figure 3 C) [13]. Radiographic measurements длины of the Ochsner's sphincter (3.20 ± 0.15 cm) were in complete agreement with the anatomical length of the sphincter described and measured by Ochsner (3.30 ± 0.15 cm) (P > 0.2). Our results were the same in length, location, and function. They have been published repeatedly in the open press [4, 12,13,14] and have not been refuted.
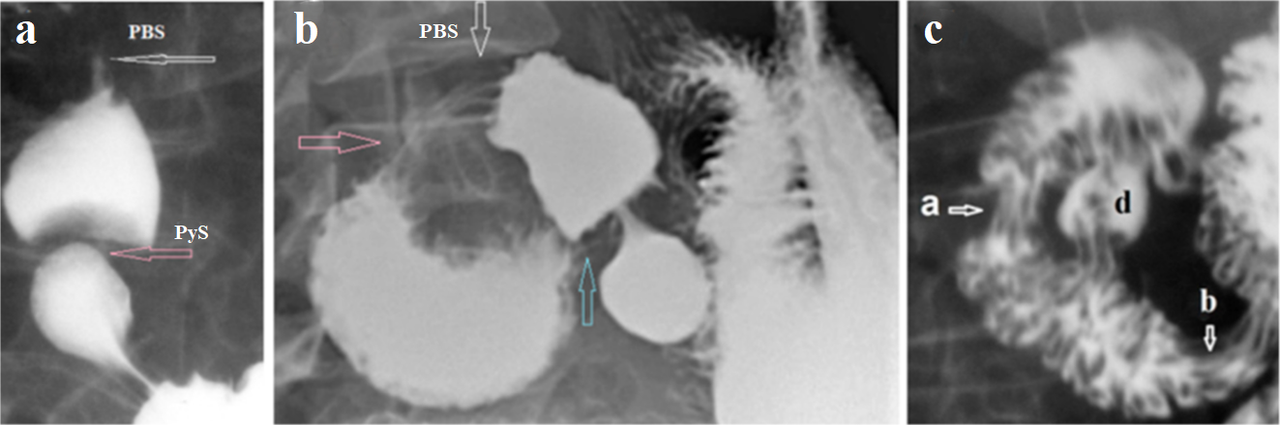
Figure 3. X-ray demonstration of the duodenal sphincters. (a) During antral contraction of the stomach, the duodenal filled to the limit, after which the pyloric sphincter (PyS) contracts, stopping the flow of barium from the stomach into the bulb. Then, during the peristaltic contraction of the bulb between the PyS and postbulbar sphincter (PBS), the pressure rises, which causes the PBS to relax, and the bolus penetrates the 2nd part of the duodenum. (b) In a patient with duodenal dyskinesia, the white arrow indicates the location of the PBS. An expansion of the duodenum is determined between the Kapanji’s sphincter (pink arrow) and the Ochsner’s sphincter (blue arrow). (c) The duodenum was emptied, but the barium remained in deep folds because the barium-filled bowel was very wide. Two zones of contraction with longitudinal folds are visible: [a] the Kapanji’s sphincter, and [b] the Ochsner’s sphincter. The juxtapapillary diverticulum [d] is located between them. These diverticula result from the extrusion of the mucosa between the muscular fibers. Thus, this diverticulum is evidence of high pressure that occurs between contracted sphincters Kapanji and Ochsner.
The above studies have shown that the Ochsner sphincter normally contracts when in contact with acid. Ochsner, during operations for duodenal and gastric ulcers, as well as for cholelithiasis, discovered hypertrophy of the Ochsner's sphincter, above which he found dilation of the duodenum, which indicated high pressure in it [4]. My research has shown that obstruction in the third part of the duodenum, which was considered the superior mesenteric artery syndrome allegedly due to compression of the duodenum between the aorta and the superior mesenteric artery, is the result of dyskinesia of the Ochsner sphincter. In all cases, the cause of dyskinesia was diseases accompanied by hypersecretion of hydrochloric acid [14, 19, 22]. These data indicate that hypersecretion of hydrochloric acid, which causes acid-related diseases, leads to duodenal dyskinesia. This is accompanied by hypertrophy of the Ochsner and Kapandji sphincters and expansion of the duodenum between them, which caused an increase in pressure in this segment where the SO opens. This is confirmed by manometric studies by Zhang et al, which found that patients with SO pathology often (36%) have duodeno-biliary reflux. In some of them (80%), the pressure in the duodenum was higher than in the common bile duct [15].
Anatomy and physiology of the biliary tract
The function of the bile ducts is to store, concentrate, and transport bile from the liver to the duodenum. To perform this function, the extra biliary tract consists of the duct system, the gallbladder, and the bile duct. The sphincter between the gallbladder and the cystic duct (Lutkens' sphincter) contracts after the gallbladder is fully filled. During its contraction, fluid is absorbed and bile concentration increases. After a meal, under the influence of cholecystokinin (CCK), the Lutkens sphincter, as well as SO, relaxes. The gallbladder contracts, and the entire portion of bile enters the duodenum. In addition to the effect of CCK, there is a reflex connection between the gallbladder and the gallbladder sphincter: an increase in pressure in the gallbladder leads to relaxation of the gallbladder sphincter and SO [16]. A peristaltic wave in the common duct conducts a bolus of bile in accordance with the law of the intestine [11]. Proximal to the bolus, the duct contracts, and caudally, the pressure decreases. The final peristaltic wave, near the SO, creates high pressure, which leads to relaxation of the SO, and the bile bolus is injected into the duodenum. In this generally accepted picture, which envisions the gradual and timely execution of each action, there is no room for retrograde peristalsis. In addition to the SO, three more sphincters have been described in the biliary tract, the presence of which has not been confirmed by other studies. However, the gallbladder sphincter (Lutkens' sphincter), whose function is unquestionable, is surprising given how minute its muscle mass can perform such an important physiological role. Figure 4 b shows an example of gallbladder dyskinesia, which manifests as swelling of the gallbladder sphincter.
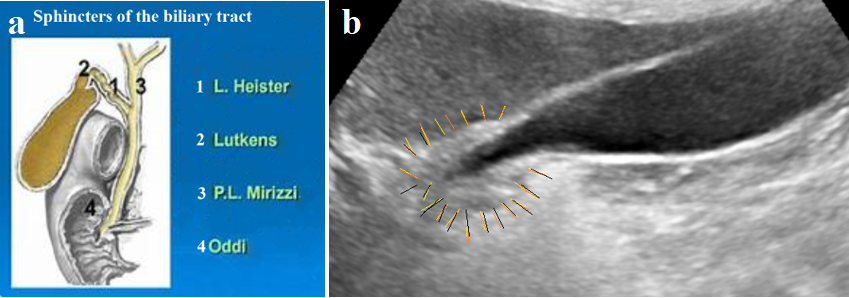
Figure 4. (a) Schematic diagram of the biliary sphincters described. (b) US gallbladder of a 78-year-old female patient with typical pain in the right hypochondrium and right shoulder, which had never occurred before. History and radiographic examination indicate mild GERD. The pain resolved spontaneously after 3 days while taking PPIs. The thickened wall at the gallbladder outlet, marked with yellow lines, indicates swelling of the gallbladder sphincter.
It is believed that in healthy individuals, most peristaltic movements are coordinated, and the direction of contractions is mostly antegrade, with only 5%-20% being retrograded [16,17]. However, endoscopic sphincter of Oddi manometry was performed in healthy volunteers. A hydraulic capillary infusion system and a triple-lumen catheter were used. The results of this study are not reliable, since it is known that up to 15% of the United States population has asymptomatic gallstones [1]. And the number of patients with biliary dyskinesia is an order of magnitude higher. Therefore, the seven control subjects cannot be considered healthy. Secondly, the infusion system inserted through the papilla of Vateri partially or completely blocks fluid passage, which disrupts the physiology of the bile ducts. Thirdly, this conclusion contradicts the law of the intestine and physiological necessity. Just as there can be no physiological reflux, physiological burp or regurgitation, there can also be no retrograde peristalsis in healthy people.
Causal relationships between biliary tract pathology and gastroesophageal reflux disease
The frequent association of calculous cholecystitis with gastric and duodenal ulcers was demonstrated in an article by Ochsner. All these observations were accompanied by hypertrophy of the wall of the third part of the duodenum, 2-4 cm in length, and dilation of the intestine proximally to this sphincter, into which the sphincter of Oddi opens. Ochsner concluded that the sphincter he described normally responds with contraction to prevent the passage of an aggressive bolus with a low pH, which can damage the jejunum. Hypertrophy of this sphincter is caused by hypersecretion of hydrochloric acid, as evidenced by gastric and duodenal ulcers [4]. Standard barium X-ray studies do not detect the sphincter, described by Ochsner. We hypothesized that Ochsner's sphincter does not contract during barium studies because barium has a high pH. We conducted a study adding 3 grams of vitamin C to a barium suspension. A decrease in pH leads to a contraction of the sphincter of Ochsner, the length of which ranges from 2 to 4.2 cm (3.2 ± 0.15 cm) [19, 20].
Hypersecretion of hydrochloric acid causes dyskinesia of the sphincter of Ochsner, manifested by hyperplasia of muscle fibers and increased spasm. This leads to increased pressure in the duodenum above the contracted sphincter. Dilation of the duodenum is evidence of this phenomenon. Dyskinesia of the sphincter of Ochsner causes two pathological phenomena: a) High pressure in the duodenum impairs bile flow, which subsequently leads to bile stagnation in the gallbladder, its concentration increases, and the formation of stones. Gradually, the common duct dilates. To overcome the high pressure in the SO and duodenum, a functional sphincter forms in the dilated common duct above the last peristaltic wave. Between it and the SO, a bilaterally closed ampulla develops. The advancing peristaltic wave increases the pressure in the ampulla, which leads to the SO opening, and the ampulla injects its contents into the duodenum. Retrograde movement in the common duct occurs only in pathological conditions. If, during contraction of the ampulla, the sphincter above the ampulla opens, unable to withstand the pressure, then the contents of the duodenum enter the common duct. This is the only pathway for microbes to enter the bile ducts, leading to acute cholecystitis. b) High pressure in the duodenum with a spasmodic Ochsner sphincter leads to duodenogastric reflux (Figure 5).
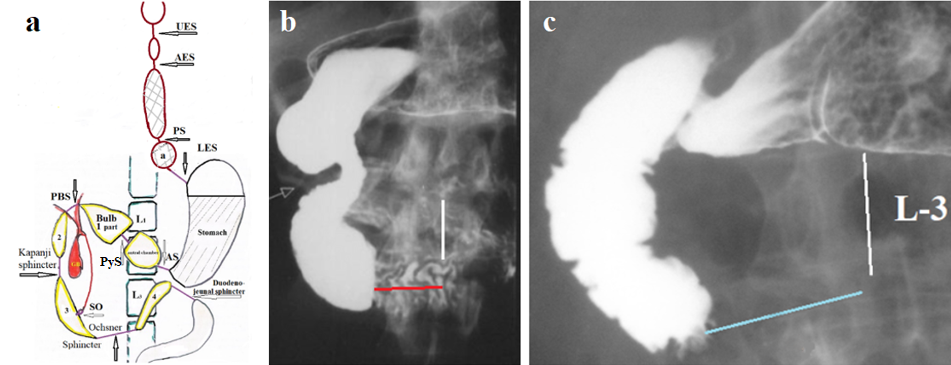
Figure 5. (a) Diagram of the sphincters of the upper gastrointestinal tract. Abbreviations: Anatomical sphincters: UES – upper esophageal sphincter; LES- lower esophageal sphincter; PyS – pyloric sphincter; SO – sphincter Oddi. Functional sphincters: AES - Aorto-esophageal sphincter; PS- Proximal sphincter; AS - Antral sphincter; PBS – Post bulbar sphincter; Kapandji sphincter; Ochsner sphincter; duodenojejunal sphincter. (b) Radiograph from the article by Neri et al., showing duodenal dyskinesia manifested by contraction of the Ochsner sphincter (red line), moderate intestinal dilation, and insufficiency of the Kapandji sphincter (arrow). Despite the absence of obstruction, the authors cited this case as a typical example of superior mesenteric artery syndrome [20,21]. (c) Contraction of the Ochsner sphincter promotes bolus reflux into the stomach. This is the mechanism for duodenogastric reflux. Our observation.
The association between biliary tract pathology and acid-related diseases is confirmed by some studies. An article by Djulai et al. demonstrated a pathogenetic link between GERD and duodeno-gastro-esophageal reflux in patients with chronic acalculous cholecystitis and cholelithiasis [22]. Study Linet al., elucidates the bidirectional causal linkages involving cholelithiasis, cholecystitis, cholecystectomy, and GERD. These results highlight the significance of GERD risk assessment in individuals suffering from biliary diseases and vice versa [18]. Our study suggests that the relationship between biliary tract pathology and acid-related diseases is underestimated. It does not consider that up to 15% of the population has asymptomatic gallstones [1]. Moreover, gallstones are the culmination of a long-term process that most often manifests after the age of 40-50 years. But the disease begins much earlier, as biliary dyskinesia [23]. Since the time when, instead of scientific research, practicing physicians determine by voting the development of gastroenterology, this pathology began to be called "functional dyspepsia." It is believed that although functional dyspepsia is mostly attributed to gastric sensorimotor dysfunctions, duodenal disturbances have also been observed. A subset of patients has duodenal mucosal inflammation, typically mild in severity [23]. The above facts indicate that hypersecretion of hydrochloric acid is an etiologic factor in the development of biliary tract pathology and, therefore, it is always combined with other acid-dependent diseases, the clinical manifestations of which are not always obvious and often the same. The pathogenesis of all acid-dependent diseases begins with a violation of the motility, which is always accompanied by varying degrees of damage to the mucous membrane [24]. Over time, functional disorders increase and anatomical changes occur (ulcers, stenosis, etc.). Pathology of the biliary system is characterized by a longer period of functional disorders, which rarely manifest themselves with symptoms, or are obscured by more intense symptoms from the stomach, duodenum, but most often by symptoms of GERD.
Etiology and pathogenesis of the biliary tract pathology
Based on the literature review and our own research, the following conclusions can be drawn. (a) Hypersecretion of hydrochloric acid, which causes acid-related diseases (esophagus, stomach, and duodenum), leads to dyskinesia of the duodenum, including the Kapanji and Ochsner sphincters with hypertrophy of their walls; (b) In the duodenum, pressure increases above the Ochsner sphincter, where the SO opens. (c) An increase in pressure in the chamber into which the SO opens leads to a disruption of its function (dyskinesia), which causes a delay in the outflow of bile and pancreatic juice. (d) Over the long term, these changes (dysmotility) are functional in nature, with minimal changes in the duodenal mucosa and dilation of common bile duct (CBD). (e) Bile retention in the gallbladder leads to increased bile concentration, which can lead to stone formation. (f) An increase in pressure in the ducts leads to a significant expansion of the CBD, a shortening of the SO occurs with the formation of an ampulla and a functional sphincter above it. (g) Duodenobiliary reflux increases pressure in the biliary system, which leads to disruption of liver function tests, chronic pancreatitis, the formation of gallstones, and acute cholecystitis, after contamination with microorganisms. (h) Pathology of the biliary system is an acid-dependent disease and therefore is always combined with other acid-dependent diseases. Their differential diagnosis can be difficult since many symptoms of different diseases are the same. (i) High pressure in the duodenum with a closed sphincter of Ochsner leads to duodenogastric reflux. Thus, the ontogenesis of the bile system disease begins from dyskinesia with the subsequent development of inflammatory, sclerotic, and anatomical changes, including the formation of ampulla, SO stenosis, metaplasia, which can lead to the tumor.
Inference
According to the philosophy of science, if a new hypothesis contradicts even one scientific fact, it must be either modified or rejected. My theoretical study is not a literature review and does not constitute a limitation, as any scientific research begins with a hypothesis. I propose a hypothesis, which does not contradict known scientific facts, but allows us to understand the causes and development of diseases of the biliary system. It will serve as a stimulus for subsequent scientific research. Only when multiple studies reveal will no contradictions with scientific data be considered a theory.
Modern research identifies several key factors that do not cause gallstone disease, but rather "influencing gallstone formation." These are scientific facts, not hypotheses. For example, cholesterol stones form because the liver secretes cholesterol, but this does not cause the stones, because cholesterol is also secreted in healthy individuals. My hypothesis doesn't deny this influence but rather explains the pathogenesis of their occurrence. For example, the concept of "microbiome" describes the presence of bacteria in stones. This is a scientific fact, not a hypothesis. The stones appear due to high pressure in the duodenum and insufficiency of the sphincter of Oddi, which leads to increased pressure in the biliary tract and stagnation of bile in the dysphunction gallbladder. This results in duodenal chyme, along with bacteria, entering the bile ducts and reaching the gallbladder using retrograde peristalsis. Impaired gallbladder contractility (scientific fact) occurs because of increased pressure in the bile ducts. A genetic factor may be associated with hypersecretion of hydrochloric acid, for example, in lactose intolerance. The shared genetic basis underlying the relationship between cholelithiasis and GERD is more significant than described in the literature [18, 22]. First, 16% of patients with an endoscopic diagnosis of GERD consider themselves healthy. Second, gallbladder disease is not limited to the presence of stones. In a significant number of patients, especially in the early stages of the disease, it manifests as gallbladder dyskinesia. This broad association of biliary disease with other acid-related diseases is consistent with my proposed pathogenesis hypothesis. Thus, my statement that hydrochloric acid hypersecretion is the cause of biliary disease consistent with scientific data and deserves further testing.
CONCLUSION
Based on a literature review and our own research, a hypothesis for the etiology and pathogenesis of inflammatory diseases of the biliary system is presented. Evidence is presented that hypersecretion of hydrochloric acid is the primary etiologic factor, suggesting that other acid-related diseases of the esophagus, stomach, and duodenum are associated to varying degrees with biliary pathology. The disease progresses over time, from impaired motor function to stone formation and purulent inflammation. In childhood and adolescence, when only motor function is impaired, biliary pathology does not manifest clinical symptoms. It is likely that in some cases, symptoms of lesions in other parts of the intestine mask biliary pathology. Discussion of the proposed hypothesis will allow for the optimization of the diagnosis and treatment of biliary diseases.
REFERENCES
- Jones MW, Kashyap S, Ferguson T. Gallbladder Imaging. (2022). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Di Ciaula A, Wang DQ, Portincasa P. (2018). An update on the pathogenesis of cholesterol gallstone disease. Curr Opin Gastroenterol. 34(2):71-80.
- Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, et al. (2007). Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 14(1):15-26.
- Ochsner AJ. (1906). VIII. Construction of the Duodenum Below the Entrance of the Common Duct and Its Relation to Disease. Ann Surg. 43(1):80-87.
- Horiguchi S, Kamisawa T. (2010). Major duodenal papilla and its normal anatomy. Dig Surg. 27(2):90-93.
- Geenen JE, Hogan WJ, Dodds WJ, Stewart ET, Arndorfer RC. (1980). Intraluminal pressure recording from the human sphincter of Oddi. Gastroenterology. 78(2):317-324.
- KUNE GA. (1964). SURGICAL ANATOMY OF COMMON BILE DUCT. Arch Surg. 89:995-1004.
- Habib FI, Corazziari E, Biliotti D, Primerano L, Viscardi A, Speranza V, et al. (1988). Manometric measurement of human sphincter of Oddi length. Gut. 29(1):121-125.
- Funch-Jensen P, Kruse A, Ravnsbaek J. (1987). Endoscopic sphincter of Oddi manometry in healthy volunteers. Scand J Gastroenterol. Mar;22(2):243-249.
- Horiguchi S, Kamisawa T. (2010). Major duodenal papilla and its normal anatomy. Dig Surg. 27(2):90-93.
- Levin MD. (2023). Gastrointestinal Motility and Law of the Intestine. (Preprint). DOI: 10.20944/preprints202312.2003.v1.
- Aldot G, Kapandji M, Ringendach J. (1956). Physiology of timed duodenal intubation. II. Role of Ochsner's sphincter in the mechanism of normal duodenal intubation and in that of certain prolongations of so-called Oddi's closed time. Arch Mal Appar Dig Mal Nutr. 45(12):449-457.
- Levin MD, Korshun Z, Mendelson G. (2016). [Duodenal motility in norm and in some diseases. Hypothesis]. Ter Arkh. 88(4):68-74.
- Levin MD. (2024). Superior Mesenteric Artery Syndrome Results From Hypersecretion of Hydrochloric Acid. (Preprint). DOI:10.20944/preprints202401.0605.v1.
- Zhang ZH, Wu SD, Wang B, Su Y, Jin JZ, Kong J, et al. (2008). Sphincter of Oddi hypomotility and its relationship with duodenal-biliary reflux, plasma motilin and serum gastrin. World J Gastroenterol. 14(25):4077-4081.
- Funch-Jensen P, Drewes AM, Madácsy L. (2006). Evaluation of the biliary tract in patients with functional biliary symptoms. World J Gastroenterol. 12(18):2839-2845.
- Funch-Jensen P, Kruse A, Ravnsbaek J. (1987). Endoscopic sphincter of Oddi manometry in healthy volunteers. Scand J Gastroenterol. 22(2):243-249.
- Lin H, Lu R, Shang Q, Gu Y, Liu Y, Yang Y, Chen L. (2025). Exploring the causal relationships between cholelithiasis, cholecystitis, cholecystectomy, and gastroesophageal reflux disease: a bidirectional two-sample Mendelian randomization study. Int J Surg. 111(1):932-940.
- Levin MD, Korshun Z, Mendelson G. (2016). Dvigatel'naya funktsiya dvenadtsatiperstnoi kishki v norme i pri nekotorykh zabolevaniyakh (gipoteza) [Duodenal motility in norm and in some diseases. Hypothesis]. Ter Arkh. 88(4):68-74.
- Levin MD. (2025). Hydrochloric acid hypersecretion is the cause of pathology of the upper digestive tract: Literature analysis. DOI: 10.32388/4QXH2Q.
- Neri S, Signorelli SS, Mondati E, Pulvirenti D, Campanile E, Di Pino L, et al. (2005). Ultrasound imaging in diagnosis of superior mesenteric artery syndrome. J Intern Med. 257(4):346-351.
- Dzhulai GS, Sekareva EV, Chervinets VM, Mikhailova ES, Dzhulai TE. (2014). [Gastroesophageal reflux disease associated with duodenogastroesophageal reflux in patients with biliary pathology: the specific features of the course and esophagogastroduodenal microbial biocenosis]. Ter Arkh. 86(2):17-22.
- Albot G, Toulet J. (1958). Duodenal or duodenobiliary dyskinesia & dyskinesia of its mesocolic digestive stage; therapeutic trial with a new 3-piperidol derivative]. Rev Prat. 8(9):989-990.
- Puthanmadhom Narayanan S, Linden DR, Peters SA, Desai A, Kuwelker S, O'Brien D, Smyrk TJ, et al. (2021). Duodenal mucosal secretory disturbances in functional dyspepsia. Neurogastroenterol Motil. 33(1):e13955.